Agenda 2025
Agenda 2025
With an annual additional investment of $53 million and fresh policy settings, HIV transmission could be ended within the next term of parliament. This statement calls for investment in prevention, testing and treatment, along with a renewed campaign against the stigma associated with HIV.

Australia can end HIV transmission by 2025



If we renew policy and investment


So that by 2030 we will avert thousands of HIV transmissions and free up health resources



Ending HIV transmission in Australia
Australia can end HIV transmission by 2025 and achieve virtual elimination. This historic achievement will only happen with a clear plan, re-focussed policy commitments and sustained effort. Agenda 2025 is our plan to achieve this goal.
Defining Elimination
Agenda 2025 adopts the UNAIDS definition of HIV elimination: a 90% reduction in Australian infections compared to a 2010 baseline. Australia has extremely low rates of HIV in sex workers and people who inject drugs and has virtually eliminated mother-to-child transmission. Two-thirds of new HIV diagnoses are in gay, bisexual and other men who have sex with men.
Leaving no one behind
The rate of HIV among Aboriginal and Torres Strait Islander people is above that of Australian born non-Indigenous people. Additionally, an increasing proportion of HIV diagnoses are among people born overseas. Eliminating HIV means we must reach all those affected, including people from priority populations, women and heterosexual men with HIV.
Executive Summary
In May 2021, Health Equity Matters (formerly AFAO) convened an expert panel of Australia’s most senior scientists, clinicians, and community leaders to review the evidence and set new targets and priorities to see Australia achieve the virtual elimination of HIV transmission by 2025. This technical paper provides the evidence assembled by the panel and priorities and targets they have endorsed to achieve virtual elimination.
The expert panel has, for the first time, endorsed a measurable target for the achievement of virtual elimination of HIV transmission in Australia. This target is a 90% reduction in HIV diagnoses in Australia (compared to a 2010 baseline). The expert panel therefore confirms that Australia will have achieved virtual elimination when less than 91 local cases are reported each year.
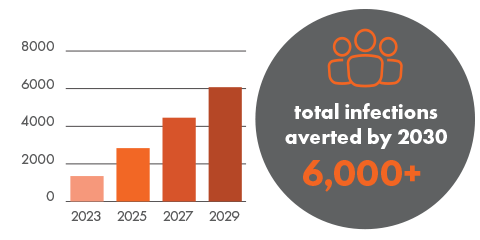
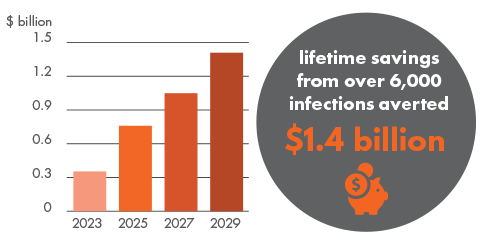
If the number of HIV diagnoses in Australia continues to 2030 at 2019 levels, 9,010 people will acquire HIV. The cost of the status quo in lifetime HIV treatment and care alone is $2.1b. By implementing the priorities set out in this paper and achieving virtual elimination by 2025, Australia will prevent over 6,000 people from acquiring HIV by 2030. By this time, Australia will have avoided $1.4b in HIV treatment and care costs.
 Prevention
Prevention
Australia has made rapid progress in scaling up HIV prevention strategies to priority populations, however there is still work to be done. PrEP has been proven to work, yet not all people at risk of HIV have access to it. By removing barriers to prevention and ensuring all communities are covered, we can ensure current measures are more effectively used to eliminate HIV transmissions by 2025.
Sustain gains and drive further reductions through community-led campaigns and peer education.
![]() $20m pa
$20m pa
PrEP and postexposure prophylaxis (PEP) available over the counter at pharmacies.
![]() $0
$0
Provide subsidised HIV pre-exposure prophylaxis (PrEP) to all who can benefit from it, regardless of visa status, on public health grounds.
![]() <$10m pa
<$10m pa
Establish minimum service levels and a national partnership agreement with States and Territories for community-led education and services, surveillance and public sexual health care.
![]() Subject to negotiation
Subject to negotiation
 Testing
Testing
Science and technology have outpaced regulation around testing. Agenda 2025 is calling on the Federal Government to take a fresh approach to HIV testing which speeds up the approval and funding of new innovations such as HIV self-testing and rapid point of care testing so those people who can benefit from this technology can access it faster.
Allow the sale of registered HIV self-tests in pharmacies and other appropriate retailers.
![]() $0
$0
Create an MBS item for rapid HIV testing so doctors can give initial results while awaiting lab confirmation.
![]() As per Medical Services Advisory Committee advice.
As per Medical Services Advisory Committee advice.
Create a Medicare Benefits Schedule (MBS) item so clinicians can provide patients with an HIV self-test they can use at home between clinical visits.
![]() As per Medical Services Advisory Committee advice.
As per Medical Services Advisory Committee advice.
Offer HIV testing on an opt-out basis when blood is drawn in settings where undiagnosed HIV is likely to be higher.
![]() $0
$0
 Treatment
Treatment
If Australia is to eliminate HIV transmission by 2025, we must ensure all people living with HIV have access to treatment. This can be achieved for $30 million by removing co-payments and providing it to all regardless of visa status. Medical Benefits Schedule (MBS) reimbursements would also increase to encourage doctors to register to treat HIV.
Remove Pharmaceutical Benefits Scheme co-payments for HIV treatment on public health grounds, consistent with other STIs, TB and serious vaccine preventable disease.
![]() $1.55m pa
$1.55m pa
Develop models for peer-led contact tracing and wrap-around clinical and peer support at diagnosis.
![]() $0
$0
Establish a priority track for the registration and funding of tests and medicines needed for public health.
![]() $0
$0
Extend HIV treatment and clinical care to all people with HIV in Australia, regardless of visa status, on public health grounds.
![]() $12m pa
$12m pa
 Stigma
Stigma
Research shows stigma around HIV/AIDS remains a barrier to accessing care and support. Agenda 2025 calls for a $9 million investment in targeted education programs in health care settings. This would fund a media program to positively engage journalists and influencers and research to better monitor HIV stigma and build evidence for effective interventions.
Establish an inter-governmental taskforce with support from the Australian Law Reform Commission to decriminalise HIV and remove visa conditions contrary to public health.
![]() $0
$0
Establish an HIV media program to positively engage journalists, digital content developers and influencers to tackle stigma.
![]() $1m pa
$1m pa
Fund foundational and implementation research to better understand and monitor HIV stigma and build evidence for effective interventions.
![]() $5m pa
$5m pa
Implement targeted education programs to reduce stigma in settings where it is especially acute (eg dentistry, other health care settings etc).
![]() $3m pa
$3m pa

Investment required $53m
In addition to a National Partnership Agreement with the States and Territories, an investment of $53 million per year is required to achieve the goal of Agenda 2025.
Elimination of HIV transmission
A reduction in HIV incidence in gay, bisexual and other men who have sex with men to less than one per 1,000 per year is the pathway to elimination of HIV transmission in Australia by 2025.
Targets
95% of people living with HIV are diagnosed
95% of people at risk of HIV infection use one or more forms of effective HIV prevention
98% of diagnosed people living with HIV are on treatment
95% of people living with HIV report no stigma in the last 12 months
Infections averted
Total savings
Making it work


Government leadership:
Committing to Agenda 2025 to provide policy and funding certainty for the HIV partnership.


Community action:
Mobilising communities, activating expertise and implementing innovations with new investment from the Commonwealth, States and Territories.


Centring populations :
Supporting people living with HIV and those at risk to remain mobilised to achieve our goal.


Clinical response:
Building the workforce to provide the world’s best treatment and care, including for those with complex social needs and co-morbidities.
Research expertise:
Investing in research to guide implementation and surveillance to know the plan is on track.