Sexually transmissible infections among young people in Australia: an overview
Sexually transmissible infections among young people in Australia: an overview
HIV Australia | Vol. 11 No. 1 | March 2013
By MELANIE MIDDLETON and ANN MCDONALD
In this article, the Kirby Institute provides a snapshot of the latest surveillance data on sexually transmissible infections (STIs) and HIV among young people in Australia.
Although rates of HIV among young people are increasing in many parts of the world, in Australia the data indicate that sustained and increasingly high rates of STIs among young people are a more immediate concern. However, the data also reflects a small increase in HIV among young men who have sex with men (MSM), indicating that this issue does need to be focused on among this population.
Introduction
A variety of socio-cultural factors such as increased duration between sexual debut and the formation of long-term partnerships, low rates of condom use and poor access to services, make young people vulnerable to sexually transmissible infections (STIs).1 As such, young people were named as a priority group in the 2010 National Sexually Transmissible Infections Strategy.
This article provides an overview of national trends in four notifiable STIs: chlamydia, HIV, gonorrhoea and infectious syphilis. More detailed analyses and information on surveillance methodology can be found in the 2012 issue of HIV, viral hepatitis and sexually transmissible infections in Australia Annual Surveillance Report, published by the Kirby Institute.
Chlamydia
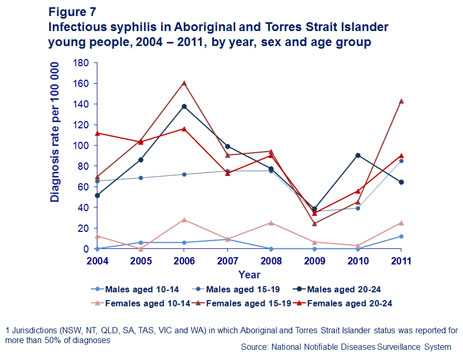
The number of diagnoses of chlamydia and the chlamydia diagnosis rate per 100,000 male and female population in the age groups 10–14 years, 15–19 years and 20–24 years, increased every year over the past ten years, from 2002 to 2011 (Figure 1).
Diagnoses were more frequent in women than men, with two infections reported for every 100 women aged 15–24 years compared to one for every 100 men in the same age group. The rate of chlamydia diagnosis among males in the age group 20–24 years was at least double the rate among males in the age group 15–19 years throughout the past ten years.
In the years from 2007 to 2011, the rate of chlamydia diagnosis among females in the 15–19 year age group increased relative to that in the 20–24 year age group, resulting in females in the age group 15–19 years recording the highest rate of chlamydia diagnosis in 2010 and 2011.
Notification rates among people aged 15–19 years were broadly similar in most states and territories, with the highest rates found in jurisdictions with a higher proportion of Aboriginal and Torres Strait Islander people, reflecting a rate of infection in those communities that is four times higher than the national average.
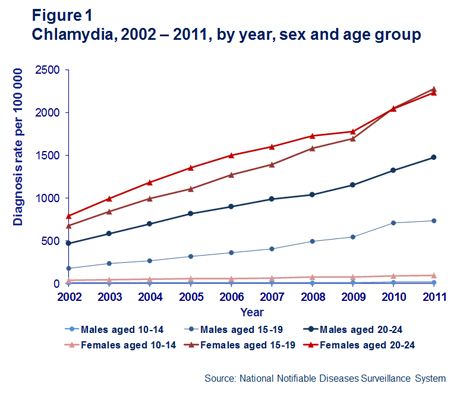
Consistent with trends in the general population, the rate of notification has increased more than three fold over the past 10 years. However, when notification data was combined with testing data from Medicare, the proportion of positive tests has remained stable at around 15% for the past five years (Figure 2), suggesting that the incidence of infection has not increased during this time despite the increasing number of diagnoses.
Data from sentinel surveillance in sexual health clinics supports this, with the proportion of heterosexual men and women aged less than 25 years diagnosed with chlamydia remaining stable over the same timeframe.2
Gonorrhoea
By contrast to chlamydia, gonorrhoea affects two distinct population sub-groups rather than the general population: men who have sex with men and Aboriginal and Torres Strait Islander people.
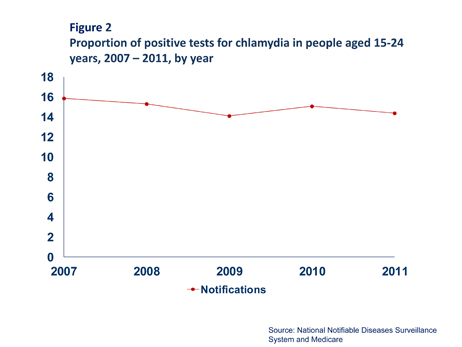
In young people, the highest rate of gonorrhoea diagnosis was in men aged 20–24 years followed by women aged 15–19 years (Figure 3).
In 2011, the largest number of notifications (1,260) was in non-Indigenous men, but the highest rate of diagnosis was in Aboriginal and Torres Strait Islander women aged 15–19 years. The rate of diagnosis in Aboriginal and Torres Strait Islander men and women aged 15–24 years was more than 30 times higher than the rate in non-Indigenous men and women of the same age (Figure 4).
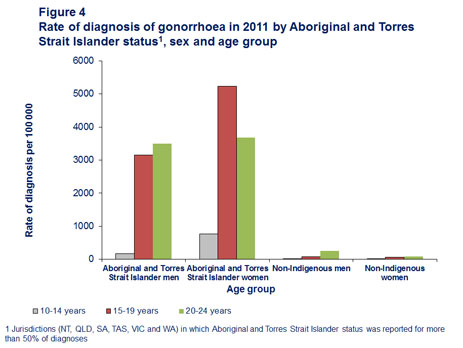
In the Aboriginal and Torres Strait Islander population, diagnoses were more frequently made in women than in men and in women aged 15–19 years than in women aged 20–24 years, a trend that was reversed in men, suggesting that a heterosexual mode of transmission predominates for this population.
The rate of diagnosis in non-Indigenous men aged 20–24 years was three times higher than the corresponding rate for women, indicating that a substantial number of infections in this population are in men who have sex with men.
Infectious syphilis
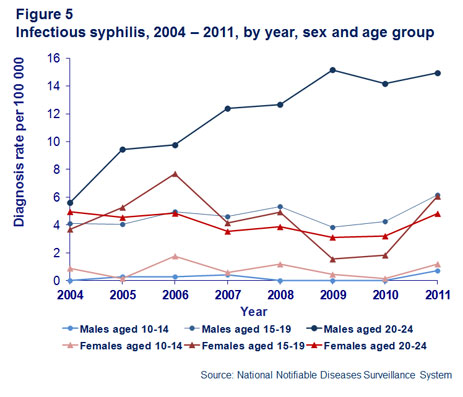
Infectious syphilis is not for the most part a disease affecting young people. In 2011, only 20% of cases occurred in people aged less than 25 years and almost half of these cases were in men aged 20–24 years of age. The rate of notification almost doubled between 2004 (3.2 per 100,000 people) to 2011 (5.9 per 100,000 people). Again, this was due to the influence of diagnoses in men aged 20–24 years reflecting the ongoing epidemic in men who have sex with men that began early last decade (Figure 5).
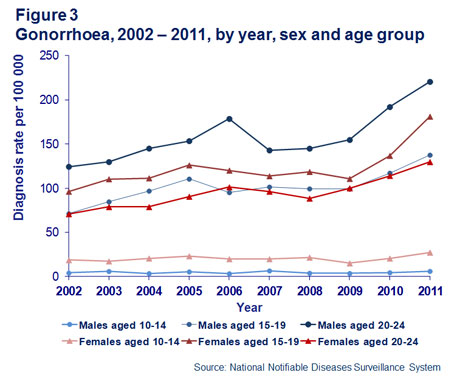
Though the overall rate of infectious syphilis for Aboriginal and Torres Strait Islander young people is significantly lower than other STIs, it is still many orders higher than the rate in non- Indigenous populations (Figure 6).
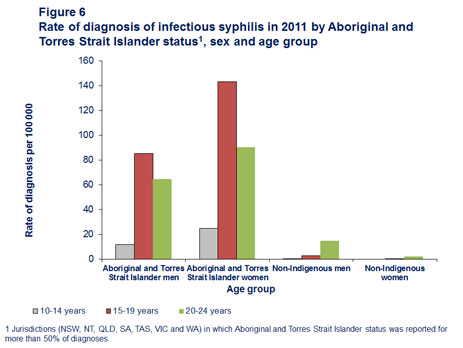
Unlike men who have sex with men, there has not been a sustained outbreak of infectious syphilis in young Aboriginal and Torres Strait Islander people in recent years. The rate is highest among women aged 15–19 years, with peaks in 2006 and 2011 indicating outbreaks in this population in those years (Figure 7).
HIV
Over the past ten years, from 2002 to 2011, 982 cases of HIV infection were reported in Australia among people aged 10–24 years at HIV diagnosis (Table 1).
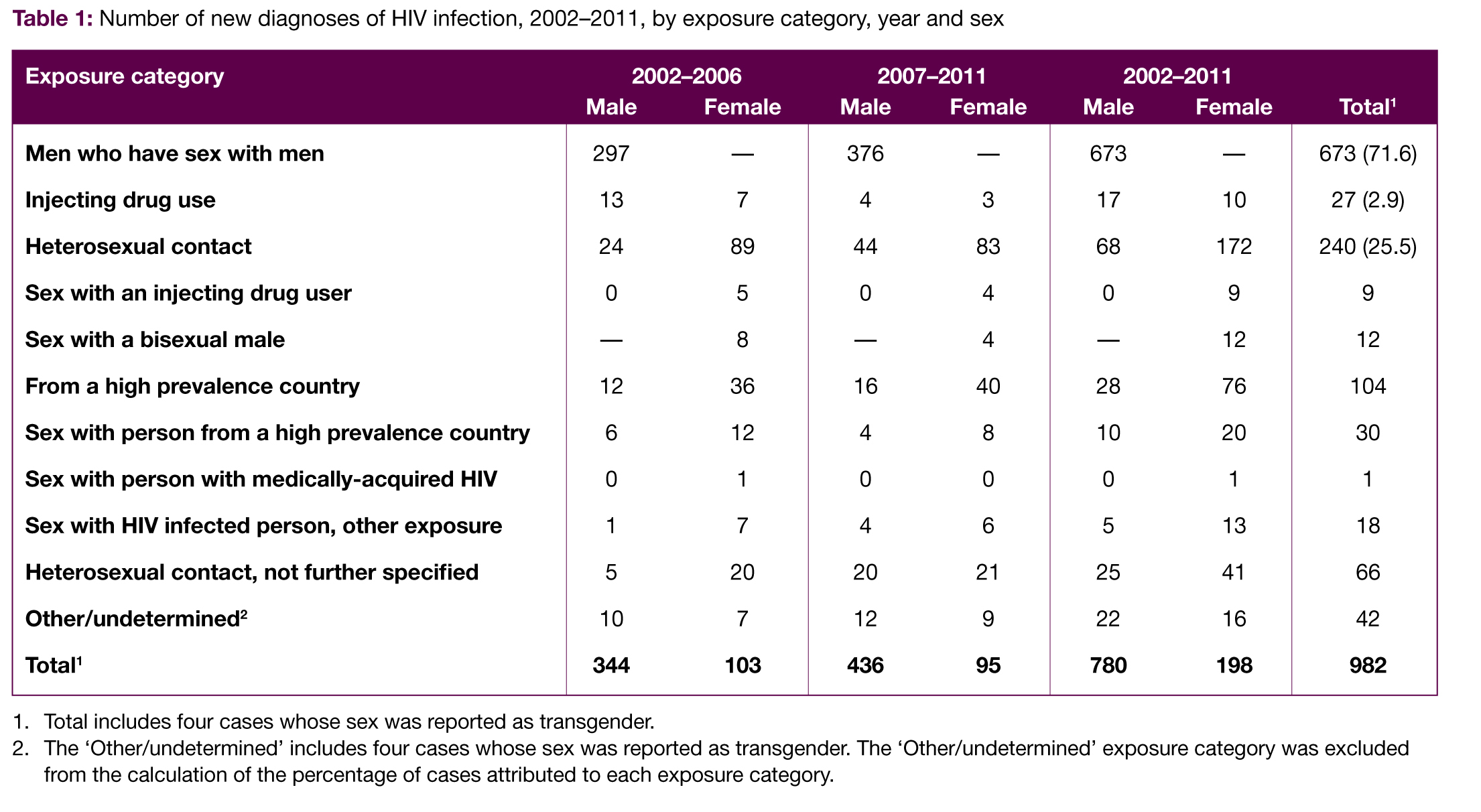
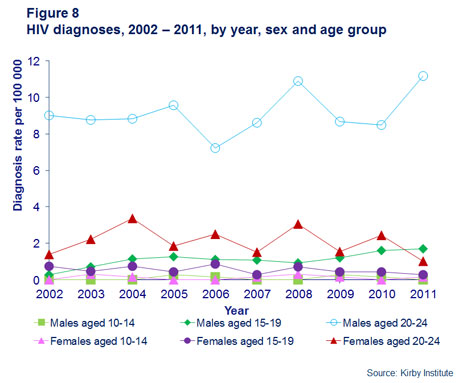
Among males, the age specific rate of HIV diagnosis in the age group 20–24 years was stable at around 8.8 per 100,000 population in 2002–2011 and was approximately seven times the rate in the age group 15–19 years (Figure 8). The rate of HIV diagnosis among females in the 20–24 year age group declined from 2.2 per 100,000 in 2002–2006 to 1.6 in 2007–2011.
Conclusion
Continuing high rates of diagnosis of chlamydial infection and diagnoses of gonorrhoea and infectious syphilis among specific population subgroups of young people in Australia indicates a need for the development of preventive interventions tailored for a young, newly sexually active population.
References
1 DiClemente, R., Crittenden, C., Rose , E., Sales, J., Wingood, G., Crosby, R., et al. (2008). Psychosocial predictors of HIV-associated sexual behaviors and the efficacy of prevention interventions in adolescents at-risk for HIV infection: what works and what doesn’t work?. Psychosomatic Medicine, 70(5), 598–605. doi: 10.1097/PSY.0b013e3181775edb
2 The Kirby Institute. (2012). HIV, viral hepatitis and sexually transmissible infections in Australia Annual Surveillance Report 2012. The Kirby Institute, The University of New South Wales, Sydney. Retrieved from: www.kirby.unsw. edu.au
Ann McDonald is Senior Research Officer, Surveillance and Evaluation Program Public Health, at the Kirby Institute. Melanie Middleton is Research Assistant, Surveillance and Evaluation Program Public Health, at the Kirby Institute.