People on the move: implications for meeting Australia’s 95:95:95 targets by 2022
By Dr Roanna Lobo, Corie Gray, and Gemma Crawford
With over one billion people moving across the world in 2018 [1], mobility is an increasingly important driver of infectious diseases including HIV. The way we conceptualise and respond to HIV in migrant and mobile populations is a global challenge. This is in part because mobility is continuous and complex, and does not by itself, or always, increase HIV risk. Gaps remain in the available data for migrant and mobile populations related to behavioural, social, political, economic and environmental risk factors. To enable effective, tailored responses for populations at risk of HIV acquisition, these must be addressed.
A global health issue
Recently, there has been significant attention paid to the complexities and subsequent challenges of increases in HIV associated with mobility. The Lancet Commission on Migration and Health [1], released in 2018, highlighted that migrants were at heightened risk for HIV compared to non-migrants. Other international organisations have also acknowledged mobile and migrant populations as priority populations for HIV, including the United Nations via the Political Declaration on HIV and AIDS (2016) [2], UNAIDS via the 2014 Gap Report [3] and in the work of the International Office of Migration [4]. These organisations, among others, provide guidance on the global and local responses needed to address HIV and mobility. All have consistent messages about targeting mobile groups in local responses and ensuring programs are responsive to the unique needs of mobile populations.
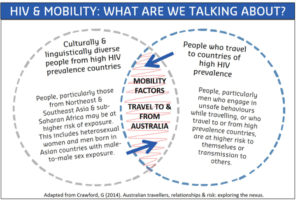
The UNAIDS report ‘Fast-Track: Ending AIDS by 2030’ in 2014 set an ambitious goal of achieving the 95:95:95 targets[5]. This means: 95% of people living with HIV knowing their HIV status; 95% of people who know their status on treatment; and 95% of people on treatment with suppressed viral loads. Australia has implemented these goals at a domestic level through the Eighth National HIV Strategy, with a timeframe of 2022. This Strategy also includes culturally and linguistically diverse people from high HIV prevalence countries, people who travel to these countries, and their partners as priority populations [6].
An effective Australian response will need to include programs at a local and regional Asia-Pacific level, acknowledging that place of HIV acquisition can be in Australia or during travel or migration overseas, and that there are multiple points for intervention, before, during and after travel or migration. Further, Australia has an important role to support the advocacy efforts of its neighbours in the region to implement healthcare systems that support universal access to testing, prevention and treatment and abolish stigmatising and detrimental laws and policies which may facilitate HIV acquisition or punish those who acquire HIV. This has mutual benefits for all countries in the region since mobility drives transmission of infectious diseases across borders.
Recognising complexity
‘Mobile populations’ is a broad term gaining currency which includes people across a range of genders, cultures, countries of birth, ethnicities, and legal statuses, with diverse experiences. The commonality amongst these populations is geographical or population mobility. This nomenclature itself is broad and highly variable, often making it difficult to categorise different types of mobility. The reasons and motivations for movement, the type of movement (e.g. short-term travel, permanent residency, etc.), origin and destination of migrants and travellers, all influence HIV risk or vulnerability, with some mobile populations at greater risk than others.
The enormous diversity within the Eighth National HIV Strategy’s priority populations requires a range of targeted responses. This includes responding to increased notifications among people from countries that do not have a high HIV prevalence as defined by UNAIDS, for example some countries in Southeast Asia, and reducing the rate of undiagnosed HIV, estimated to be more than 25% among people born in Southeast Asia who are living in Australia [7].
What do we know about mobile populations’ experiences of HIV risk and prevention?
Australia’s approach to HIV prevention must be grounded in evidence and responsive to changes in epidemics. According to national surveillance data, during the period 2014-2017, 49.6% of people describing heterosexual exposure were reported to have acquired HIV overseas [7]. In Western Australia (WA), a large majority of heterosexual men who acquired HIV in Southeast Asia were Australian-born, while male and female HIV acquisition in sub-Saharan Africa was typically heterosexual exposure among people born in that region [8]. In Victoria (VIC), almost half of the migrants (46%) diagnosed with HIV between the period of 2005 to 2014 acquired their HIV after migration, indicating a need for Australian-based prevention for migrant populations [9].
Nationally, by region of birth, HIV notification rates were highest among those from the Americas (13.5 per 100,000), Northeast Asia (4.8 per 100,000), Southeast Asia (14.0 per 100,000) and sub-Saharan Africa (13.1 per 100,000) [7]. Rates have remained relatively consistent in Australia since 2008 (3.2 per 100,000). The proportion of newly diagnosed men reporting sex with men, who were born in Southeast Asia, Northeast Asia, and Southern and Central Asia, has more than doubled in the past ten years [7]. In the most recent quarterly surveillance report for New South Wales (NSW), 52% (n=32) of new HIV diagnoses were among overseas born men who have sex with men (MSM), with a large proportion of these men born in Asia. This was 10% more than the preceding five year mean and exceeded the number of HIV diagnoses in Australian born MSM [10].
How do we respond to these differences?
While available surveillance data provide some insights into who may be mobile, they also conceal differences. For example, migrant communities of interest are frequently defined by country of birth, or language spoken at home, however country of birth is not always specified in regional surveillance data. This makes it difficult to identify specific groups within these communities who are at increased risk of HIV, and which other factors are likely to contribute to HIV risk. These may include factors such as visa status; residency or citizenship; ethnicity; access to health services (Medicare eligibility, international students overseas health insurance, private health insurance); English proficiency; income; number of partners; frequency and length of travel; social networks; peer influence; sexual networks; access to health promotion and prevention messages; experiences of stigma, discrimination and racism. The data available for travellers are also limited, in particular our understanding of risk; social networks; peer influence; income; health status; social connectedness; and support.
An additional consideration for health system and public health policy, practice and research is that in many cases, prevention work is attempting to engage groups within a wider group, such as Asian MSM amongst the broader MSM population. This intersectionality introduces a further level of complexity and, in some populations, other factors that influence risk, for example power, discrimination and oppressive institutions.
Efforts to improve available behavioural surveillance will improve access to community-level data and our ability to deliver targeted interventions. This work includes harmonising national surveillance data across states and territories, and an Australian Research Council Linkage Project to develop a periodic survey of culturally and linguistically diverse (CaLD) migrants to better understand the factors that predict poor health outcomes related to blood-borne viruses and sexually transmitted infections. Without such data, assumptions are made about who is at risk and what their risk factors are. These assumptions then drive prevention messages. The emphasis may be on short term, single strategies such as social marketing campaigns for travellers, or the translation of resources for CaLD groups without subsequent monitoring of behaviour change.
What is being done to address HIV and mobility in Australia?
In 2014, the HIV and Mobility in Australia: Road Map for Action was published. The Road Map sought to capture the unique needs of people travelling to and from high HIV prevalence regions and Australia. It shone a spotlight on the context and types of mobility and differences in HIV diagnoses across Australia relating to mobile populations. In addition, the report provided a comprehensive implementation plan to operationalise Australia’s HIV response and stressed the need for more targeted and nuanced responses. At the time, the authors wrote a piece for HIV Australia about the impact that population mobility has had and will continue to have on HIV epidemics around the world including in Australia [11].
Four years on, and with the release of the Eighth National HIV Strategy, the authors thought it was timely to reflect on the challenges and successes of efforts to address issues of population mobility and HIV here in Australia at a local and national level.
The HIV and Mobility in Australia: Priority Actions (https://siren.org.au/hiv-mobility/community-of-practice-for-action-on-hiv-and-mobility/priority-actions/) [12] was released in 2018 following further consultation with the HIV sector and a review of the most recent literature and epidemiology. This document provides additional impetus for action in six priority areas, building upon the Road Map for Action, to operationalise the Australian response to HIV and mobility and future iterations of national and jurisdictional policies relating to HIV.
We also asked members of the Community of Practice for Action on HIV and Mobility (CoPAHM) https://siren.org.au/hiv-mobility/community-of-practice-for-action-on-hiv-and-mobility/) in South Australia (SA), WA, VIC and Queensland (QLD) to reflect on local achievements to date and the issues they see as most pressing in addressing HIV in mobile and migrant populations.
Six priority actions for HIV and Mobility in Australia
- Local solutions
Relevant jurisdictions to plan and implement state-specific responses to HIV in migrant and mobile populationsAchievement
“State-wide collaboration including the SA CoPAHM workshop in 2017 and resulting SA summary of priority actions, many of which have been integrated in to annual work plans for STI and HIV funded NGOs in SA.”
– Holley Skene (Communicable Disease Control Branch, Viral Hepatitis STI & BBV
section, SA Health) - Health literacy
Increase health literacy and know how to access combination prevention strategies availablePressing issue
“PrEP is working but we still need to promote condom use in CALD as the main prevention method”
– Zhihong Gu (Ethnic Communities Council of Queensland) - Test
Understand and reduce barriers to HIV testing and make new testing technologies widely availablePressing issue
“Should a national stigma campaign be funded, we need to ensure that it not merely includes but centres migrant and mobile populations. This includes in its messaging, imagery and dissemination. Crucially, it also must involve PLHIV from priority migrant populations AND community leaders/ ethnic community organisations to ensure the context, purpose and messaging is culturally safe.”
– Jen Johnson (La Trobe University) - Treatment and prevention medication
Advocate for the inception of a policy mechanism to provide access to HIV treatment and HIV Pre-Exposure Prophylaxis (PrEP) for temporary visa holders who are ineligible for MedicarePressing issue
“[We need to see] access to HIV treatment and PrEP for temporary visa holders who are ineligible for Medicare.”
– Holley Skene (SA Health) - Inform
Harmonise surveillance data reporting for both migrant and mobile populations, including sexual behaviour, testing rates, notifications, treatment initiation and PrEPAchievement
“ARC Linkage Project funded to develop and test an STI/BBV behavioural surveillance survey for CALD populations and the requirements to implement the survey periodically”
– ARC Linkage Project partners (WA, QLD, SA, VIC, NSW) - Evaluate
Develop core indicators to assess effectiveness of HIV programs for mobile and migrant populationsPressing issue
“Meaningful engagement with mobile and migrant populations is required to understand program outcomes of importance to affected communities”
– SiREN (Sexual Health and Blood-Borne Virus Applied Research & Evaluation Network, Curtin University, WA)
Where to from here?
Australia has developed a successful public health approach to HIV prevention recognised internationally for its effectiveness in responding to the HIV epidemic. Key components are investment, bipartisan government support, social, behavioural and clinical research and significant involvement by affected groups. These approaches need to be applied in the context of HIV and mobility if we are to deliver on our targets of 95:95:95 [13].
A key goal in contemporary Australian HIV policy is to ‘virtually eliminate’ HIV transmissions by 2022, ensuring ‘no one is left behind’. The Eighth National HIV Strategy reaffirms this approach. Despite many successes, including decreases in HIV diagnoses amongst African migrants in Australia and subsidised access to PrEP and effective treatment for people with HIV through the Pharmaceutical Benefits Scheme, challenges remain.
The movement of people will continue to increase globally. There is a need for health systems to adapt and for greater political will and cross-border collaboration to ensure equitable access to HIV prevention, testing and treatment for all people living in Australia or travelling to and from Australia to regions of high HIV prevalence.
References
- Abubakar, I.; Aldridge, R.W.; Devakumar, D.; Orcutt, M.; Burns, R.; Barreto, M.L.; Dhavan, P.; Fouad, F.M.; Groce, N.; Guo, Y. The UCL–Lancet Commission on Migration and Health: the health of a world on the move. The Lancet 2018, 392, 2606-2654, doi:10.1016/S0140-6736(18)32114-7.
- United Nations. Political Declaration on HIV and AIDS; United Nations: New York, USA, 2016.
- UNAIDS. The Gap Report; UNAIDS: Geneva, Switzerland, 2014.
- International Organization for Migration. HIV and Population Mobility; IOM: Geneza, Switzerland, 2010.
- UNAIDS. Fast-Track: Ending the AIDS epidemic by 2030; UNAIDS: Geneva, Switzerland, 2014.
- Department of Health Australian Government. Eighth National HIV Strategy 2018 – 2022; Commonwealth of Australia: Canberra, ACT, 2018.
- Kirby Institute. HIV, viral hepatitis and sexually transmissible infections in Australia: Annual Surveillance Report 2018; Kirby Institute, UNSW Sydney: Sydney, 2018.
- Department of Health Western Australia. The Epidemiology of Notifiable Sexually Transmitted Infections and Blood-Borne Viruses in Western Australia 2016; Communicable Disease Control Directorate Department of Health, Western Australia: Perth, Western Australia, 2017.
- Peach, E.; Lemoh, C.; Stoove, M.; Agius, P.; El Hayek, C.; Higgins, N.; Hellard, M. Aiming for 90–90–90–the importance of understanding the risk factors for HIV exposure and advanced HIV infection in migrant populations and other groups who do not report male-to-male sex. Sexual health 2018, 15, 441-450, doi:10.1071/SH17192.
- New South Wales Health. NSW Health Strategy 2016-2020: Fourth Quarter and Annual Data Report 2017 NSW Health: NSW, 2018.
- Crawford, G.; Lobo, R.; Brown, G. HIV and mobility in Australia: Road Map for Action. HIV Australia 2015, 13, 49.
- Community of Practice for Action on HIV and Mobility. HIV and Mobility: Priority Actions.; Sexual Health and Blood-Borne Virus Applied Research and Evaluation Network, Curtin University: Perth, WA, 2018.
- Crawford, G.; Lobo, R.; Brown, G.; Maycock, B. The influence of population mobility on changing patterns of HIV acquisition: lessons for and from Australia. Health Promotion Journal of Australia 2016, 27, 153-154, doi:10.1071/HE15042.
Dr Roanna Lobo is currently the SiREN project manager and Senior Research Fellow with CERIPH in the School of Public Health at Curtin University.
Corie Gray currently works as the Coordinator for the Community of Practice for Action on HIV and Mobility (CoPAHM).
Gemma Crawford is currently Course Coordinator for postgraduate health promotion, Lecturer in the School of Public Health and Research Fellow with CERIPH at Curtin University. Gemma is the current national President for The Australian Health Promotion Association.
Additional achievements in Road Map action areas – some regional highlights
Commonwealth and state leadership
PrEP as a viable prevention tool within various CaLD communities and its mainstream use as a travel prophylactic.
Community mobilisation
SA – PEACE Forum ‘Understanding the journey of international students’. International students highlighted to service providers who attended the session their lived experience of being international students and shared their perspectives of the issues, the risk factors and what could be done to improve practice and policy to support international students.
VIC – Victorian African Health Action Network (VAHAN) works to mobilise Victorian African communities to respond to the challenges of HIV, blood borne viruses and related sexual and reproductive health issues. No organisation as yet exists to articulate the concerns of African Australian communities in the development and implementation of HIV/sexual health policy in Australia at a Commonwealth or state level. Groups like VAHAN, and similar groups in other jurisdictions, continue to play a key role in pushing for the greater and more meaningful inclusion of HIV affected African communities in Australia’s response to HIV.
Development of services for mobile or migrant populations
SA – Travel Safe campaign and booklet developed by PEACE Multicultural Services (https://www.rasa.org.au/travelling-overseas-then-plan-ahead/).
SA – Dedicated HIV Women’s Program at PEACE Multicultural Services and the associated Indaba HIV group and resources (https://indabahiv.com.au/).
Research, surveillance and evaluation
SA – Study investigating how HIV-related stigma and discrimination are experienced by people from CaLD Backgrounds. Conducted in partnership with Relationships Australia SA and involved interviews with community leaders, people from CaLD backgrounds living with HIV, and service providers from a range of health and other organisations. The study found multiple forms of stigma and discrimination experienced in CaLD communities which have important implications for health and wellbeing.
VIC – Positive Women Victoria’s Barriers and Opportunities for Meaningful Engagement: Needs of women from African diaspora communities in Victoria, Australia who are living with HIV. Led by HIV peer-based organisation, the report highlighted the importance of working with non-HIV specific clinical services, particularly when responding to women’s experiences. This study also identified opportunities for meaningful engagement with migrant and mobile populations to inform culturally appropriate and accessible service provision within the Australian HIV response.
WA – Investment in research and policy with a focus on HIV and mobility including The male overseas acquired HIV social research study led by researchers at Curtin University, University of New South Wales and La Trobe University, and continued through the HIV mobility projects at SiREN (https://siren.org.au/).
Download PDF Version: People on the move: implications for meeting Australia’s 95:95:95 targets by 2022