Improving treatment outcomes for HIV-positive Aboriginal and Torres Strait Islander people at Cairns Sexual Health using the treatment cascade as a model
Improving treatment outcomes for HIV-positive Aboriginal and Torres Strait Islander people at Cairns Sexual Health using the treatment cascade as a model
HIV Australia | Vol. 13 No. 3 | December 2015
By Morgan Dempsey, Mary Elliott, Carla Gorton, Joanne Leamy, Sara Yeganeh and Karly Scott
This article reflects the work of the multidisciplinary team of Aboriginal and Torres Strait Islander health workers, doctors, pharmacists, psychologists and nurses at Cairns Sexual Health to improve the treatment outcomes for HIV-positive Aboriginal and Torres Strait Islander people.
Our service uses the treatment cascade as a model to gauge our success in improving health outcomes for people living with HIV, as it describes the stages of health care that people living with HIV pass through, from diagnosis through to viral suppression.
Our clinic is fortunate to have an onsite pharmacy with an HIV Pharmacist and Pharmacy Assistant.
Cairns Sexual Health usually sees 12–13 new cases of HIV each year, with 1–2 cases per year among Aboriginal and/or Torres Strait Islander people.
However, in July 2014, our service began to see a spike in the number of new cases of HIV among Aboriginal and/or Torres Strait Islander men who have sex with men (MSM). This was the catalyst that drove our team to question whether we really knew our epidemic.
As a team, we believed that our service adequately met the needs of our clients in terms of engagement to service, initiation and adherence to antiretroviral (ART) treatment with achieved undetectable viral load (VL).
In 2014, our Intern Pharmacist conducted an audit (with approval from Cairns Hospital and Health Service Ethics Committee) of Aboriginal and Torres Strait Islander people living with HIV, who were attending Cairns Sexual Health.
A key question asked in the audit was, ‘Once clients reach undetectable, do they stay there?’
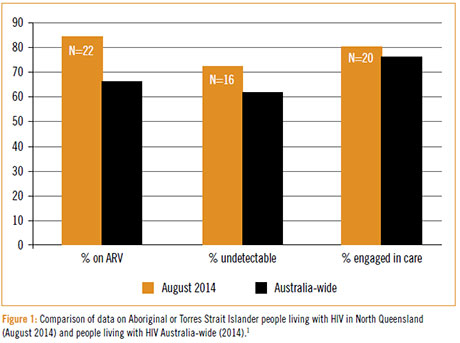
The audit identified 25 HIV-positive people who identified as Aboriginal and/ or Torres Strait Islander. Of this cohort, 22 people were receiving ART, 16 were undetectable and 20 were engaged in care.
Figure 11 compares our August 2014 figures on engagement, treatment and viral load status against Australia-wide data on people living with HIV.
By the end of 2014, Cairns Sexual Health had 15 new cases of HIV, with 6 (40%) identifying as Aboriginal and/or Torres Strait Islander men who have sex with men (MSM).
The audit also found that of these new cases, 50% where diagnosed by GP services and 33% by Aboriginal or Torres Strait Islander health care services.
Assessing the treatment cascade
We were interested to know how this cohort of people measured on the HIV treatment cascade.
The cascade is often presented as linear, where a person receives a positive HIV test result; is linked to care; begins antiretroviral treatment; maintains engagement with care and ART; and achieves viral suppression.2
However Sprague and Simon (2014)3 describe how people move in and out of the treatment cascade, rather than progress in a linear manner (see Figure 27).
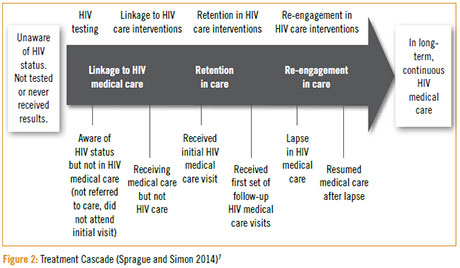
Although we perceived our service to engage this group well, the audit highlighted that this cohort appear to move in and out of the treatment cascade depending on what is happening in their lives at any given time.
We found that individuals may or may not engage in HIV care following diagnosis; may or may not begin ART; may or may not remain on ART; may disengage; and may re-engage when they become ill or are hospitalised.
Many reasons for this movement seem to be based around the social determinants of health such as culture, income, housing, education, place of birth, social exclusion, and the wider forces and systems that impact on daily life.4
We observed that the barriers5 or causes of leaks6 from the treatment cascade included: the clinic entrance; lack of transport; homelessness; lack of family awareness, no support; HIV literacy; recreational drug use; family and cultural responsibilities; hidden nature of taking ART; stigma; lack of finance; work; and new diagnosis.
Clients also stated:
- ‘I just wanted to run away’
- ‘Drugs were awful’
- ‘Am sleeping on couches’
- ‘I need to get some food now’
- ‘I live in 2 houses’
- ‘I need to feed the children’
- ‘I have a Pharmacy bill’
- ‘I live with other people’
- ‘I cannot tell my family’
- ‘Family work at health service’.
When we looked at our service, we identified our own barriers, including:
- ‘But why won’t he just take his pills?’
- ‘Disruption’ to clinic flow
- ‘He is my client’
- Inflexibility of service model
- For missed appointments, it becomes a fine line between following up or stalking!
- Lack of funding to culturally appropriate NGOs
- Lack of social infrastructure
- Need for social workers.
Our service continued to monitor how this small group of HIV-positive people move in and out of the treatment cascade over a 12-month period (see Figure 3).
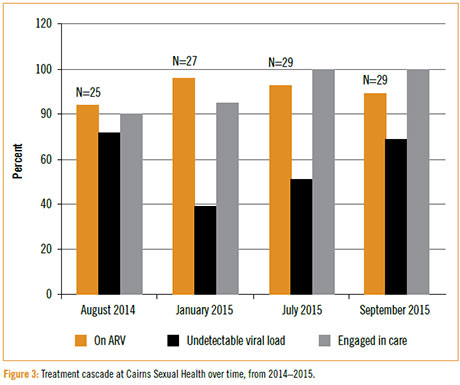
As at September 2015, our service has 29 Aboriginal and/or Torres Strait Islander HIV-positive clients, 27 of whom are male (all MSM) and 2 female.
Over the 12 months we have developed our knowledge and insight into barriers affecting engagement of Aboriginal and/or Torres Strait Islanders with HIV care.
As a team we have actively used this insight to put in place enablers to health care access, which has resulted in a dramatic shift from 80% to 100% of the cohort being engaged in care; with currently 89% on ART and 69% undetectable.
In our experience, the enablers for engaging and maintaining Aboriginal and Torres Strait Islander HIV-positive people in care are many and varied, and we needed to remain flexible.
Aboriginal and Torres Strait Islander health workers have been central to facilitating engagement, access to services, education and support, as they work in a holistic way.
Cultural protocols, men’s and women’s business, stigma, shame and being ostracised in community are contributing factors as to why Aboriginal and Torres Strait Islander people are reluctant to engage in health services for HIV treatment.
While the Aboriginal and Torres Strait Islander health workers followed cultural protocols, we sometimes found that young men preferred to engage with an older female health worker.
Some examples of enablers to health care access within our service:
- Rearranging the waiting room so that the chairs face the window rather than the entrance, improving anonymity and reducing shame
- Utilising the staff back door entrance rather than bringing reticent people through the front door, which is labelled ‘Sexual Health’
- Improving links between hospital and clinic, with clinic staff and HIV Pharmacist visiting people when they are admitted to hospital. Service includes providing information about the Sexual Health Clinic, and providing support for people newly diagnosed around HIV and ART
- Establishing a pharmacy fee waiver for ART to clients with financial problems n Providing increased flexibility of scheduling appointments
- Provision of transport to and from appointments
- As a service, we became better at ‘expecting the unexpected’
- All members of the multidisciplinary team are crucial to providing holistic care
- We provide information about different staff, which allows clients to choose who they would like to see. This has allowed clients to develop positive relationships with particular staff
- SMS was used to engage clients initially, and often we could have SMS conversations prior to meeting the client. This gave people a chance to get to know us slowly and engage on their terms. It also meant we could ascertain when it suits them for us to call so they don’t use their own phone credit. SMS is also used to remind clients of their appointments.
- We spent time supporting nonclinical staff to understand why this group of people needed extra support.
Key learning outcomes
This work has improved our knowledge of the HIV treatment cascade and of factors that enable clients to maintain engagement in care. It is important to note that people do not maintain an undetectable viral load forever.
Care by a multidisciplinary team of Aboriginal and Torres Strait Islander health workers – including pharmacists, nurses, psychologists, and doctors – is essential. Each team member needs to get to know the whole person, rather than focusing only on HIV.
Clinical services also need to provide flexible models of care. Our experience illustrates the importance of dismantling barriers as they arise, in order to keep people engaged in care.
It seemed to us that those requiring most support to engage in care, take antiretroviral treatment and remain in care were diagnosed within the last two years.
This is useful information for services to be aware of when caring for Aboriginal and Torres Strait Islander people who are newly diagnosed with HIV.
References
1 Templeton, D., Wright, S., McManus, H., Lawrence, C., Russell, D., Law, M., et al. (2015). Antiretroviral treatment use, comorbidities and clinical outcomes among Aboriginal participants in the Australian HIV Observational Database (AHOD). BMC Infectious Diseases, 15(326).
2 amfAR. (2013, December). The HIV Treatment Cascade [fact sheet]. Retrieved from: www.amfar.org
3 Sprague, C., Simon, S. (2014). Understanding HIV care delays in the US South.
Int. Journal for Equity in Health, 13(28). doi: 10.1186/1475-9276-13-28
4 Braveman, P., Gottlieb, L. (2014). The social determinants of health: it’s time to consider the causes of the causes. Public Health Reports, Supp 2 (129).
5 Yehia, B., Stewart, L., Momplaisir, F., Mody, A., Holtzman, C., Jacobs, L., et. al. (2015). Barrier and facilitators to patient retention in HIV care. BMC Infectious Diseases, 15(246). doi:10.1186/s12879-015-0990-0
6 Ayala, G., Makofane, K., Santos, G., Arreola, S., Hebert, P., Thomann, M., et al. (2014). HIV treatment cascades that leak: correlates of drop-off from the HIV care continuum among men who have sex with men worldwide. Journal of AIDS & Clinical Research, 5(8).
7 Sprague, C., et al. (2014). op cit.
Morgan Dempsey is Senior Health Worker at Cairns Sexual Health.
Mary Elliott is Pharmacist at Cairns Sexual Health.
Carla Gorton is HIV, Sexual Health and Hepatitis Coordinator at Cairns Sexual Health.
Joanne Leamy is Clinical Nurse Consultant (CNC) Contact Tracing at Cairns Sexual Health.
Sara Yeganeh and Karly Scott are Pharmacists at Cairns Sexual Health.

