Findings from the Queensland Injecting Drug Survey (QuIDS): comparing hepatitis C risk behaviours among Indigenous and non-Indigenous people who inject drugs
Findings from the Queensland Injecting Drug Survey (QuIDS): comparing hepatitis C risk behaviours among Indigenous and non-Indigenous people who inject drugs
HIV Australia | Vol. 11 No. 3 | October 2013
By Abhilash Dev1, Robert Kemp,1 James Ward,2 Suzanna Henderson,3 Sidney Williams,4 Andrew Smirnov,3 Maria Plotnikova3 and Jake M Najman3
An estimated 10,000 new hepatitis C (HCV) infections occur each year in Australia.1 It has been estimated that 91% of new HCV infections are acquired through injecting drug use.2
A good deal of what is known about the transmission of hepatitis C and injecting drug use in Australia is based upon studies of the non-Indigenous population.
Only a small number of studies have specifically recruited large samples of Aboriginal and Torres Strait Islander people who inject drugs (PWID) and few have concurrently recruited a comparison group of non- Indigenous PWID.
There is a lack of data on risk-taking behaviours among Indigenous PWID but it is generally assumed that Indigenous Australians who use injecting drugs engage in a wide range of risk taking behaviours, and that those in custody are at the greatest risk of acquiring hepatitis C.3
The Aboriginal and Torres Strait Islander population may be disproportionately represented among people who inject drugs and are over represented among the Australian prison population.
These two factors place Indigenous Australians at a higher risk of HCV transmission than others in the general population.4, 5
Current estimates suggest that the rate of HCV infections in the Aboriginal and Torres Strait Islander population is somewhere between two and ten times higher than in non-Indigenous populations.6
While further research is required to test these estimates, studying the HCV risk behaviours among the Indigenous Australian population provides an indication of the HCV (and HIV) potential in this population group.
An analysis of participants in the Australian Needle and Syringe Program Survey, conducted since 1995, found higher proportions of Indigenous than non-Indigenous participants were HCV antibody positive (57% vs 51%, p<0.001) and that Indigenous status and female gender were associated with HCV antibody seropositivity.7
The Queensland Injecting Drug Survey (QuIDS) was initiated in 2010 in response to concerns about increasing rates of injecting drug use and associated risk behaviours among Aboriginal and/or Torres Strait Islander people.
Current users of injecting drugs, defined as having injected more than once in the previous 12 months, were recruited from 12 metropolitan and regional centres throughout Queensland.
Participants were asked to complete a survey investigating patterns of drug use, risk factors, health status and health service access of current Indigenous and non-Indigenous PWID in Queensland.
QuIDS sought to examine systematic differences between Indigenous and non-Indigenous HCV-positive PWID.
In our sample of injecting drug users we investigated the social determinants, patterns of use and overall health and wellbeing of those at risk of acquiring HCV infections comparing Indigenous and non-Indigenous PWID.
Findings of the study indicated that risk factors for HCV were similar in both groups; risk factors including injecting drug use, prior use of heroin and a current custodial sentence. Indigenous adolescents showed more markers of social disadvantage and higher rates of hepatitis B than non-Indigenous offenders.8
Design and methods
QuIDS used respondent driven and peer network sampling methods to recruit 294 Indigenous and 275 non-Indigenous injectors in ten urban and regional settings across Queensland.
A number of peer interviewers were trained to recruit and interview study participants who were either known to them (convenience sample) or accessed through a systematic process of peer referral (respondent driven sampling).
Participants provided informed consent and were reimbursed $50 for their time in conducting the survey.
The starting point for the respondent driven recruitment was through Queensland Needle and Syringe Program sites at specified locations.
Findings
Table 1 sets out the QuIDS findings regarding demographic differences between Indigenous and non-Indigenous PWID.
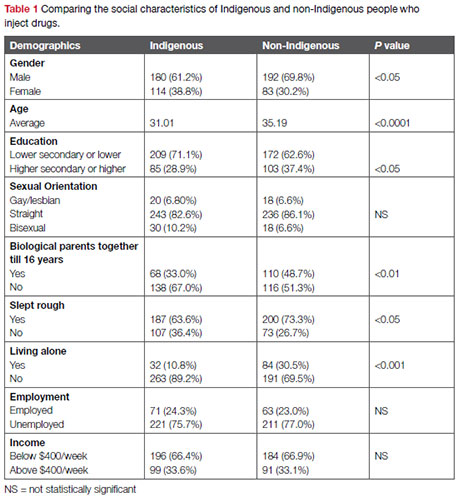
Indigenous PWIDs were slightly more likely to be female (38.8% vs 30.2%), be of younger mean age (31.0 vs 35.2 years of age), of lesser educational level (28.9% vs 37.4%), and to have had parents separated by the time they were 16 years of age (67.0% vs 51.3%).
By contrast, non-Indigenous respondents were slightly more likely to identify as heterosexual (86.8% vs 82.8%), more likely to have slept rough (73.3% vs 63.6%) and to be living alone (30.5% vs 10.8%).
On employment, income and imprisonment history Indigenous and non-Indigenous PWIDs were similar.
Table 2 suggests Indigenous PWIDs were more likely to have injected amphetamines (90.4% vs 83.5%) in the past six months, but the rates of injecting other drugs were similar.
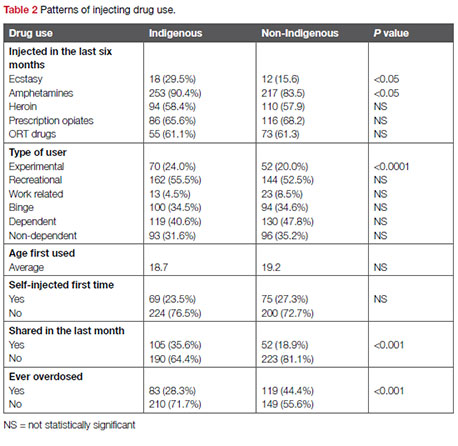
There were no differences between Indigenous and non- Indigenous respondents for reported first use of drugs, but Indigenous respondents were more likely to report that when they last injected they shared a needle (35.6% vs 18.9%).
Non-Indigenous respondents were more likely to have ever overdosed (28.3% vs 44.4%).
Table 3 examines the health history of Indigenous and non-Indigenous respondents in the sample.
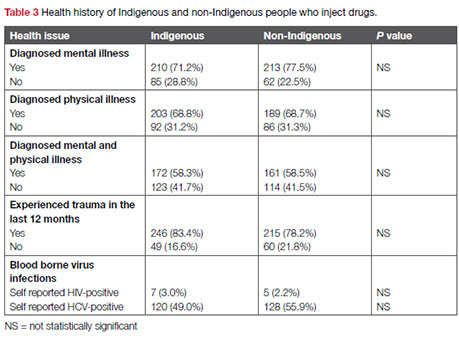
The results suggest that the two comparison groups have a remarkably similar health history, with similar levels of diagnosed self-reported mental illness (over 70% of both groups have been diagnosed with a mental illness), similar levels of diagnosed physical illness (almost 70% of both groups), and similar levels of trauma experienced in the past 12 months.
Interestingly, Indigenous and non-Indigenous respondents had low (but similar) rates of self-reported HIV-positive status (3.0% vs 2.2%), and similar levels of self-reported hepatitis C-positive status (49.0% vs 55.9%).
Table 4 compares the social characteristics of Indigenous and non- Indigenous respondents who were HCV-positive.
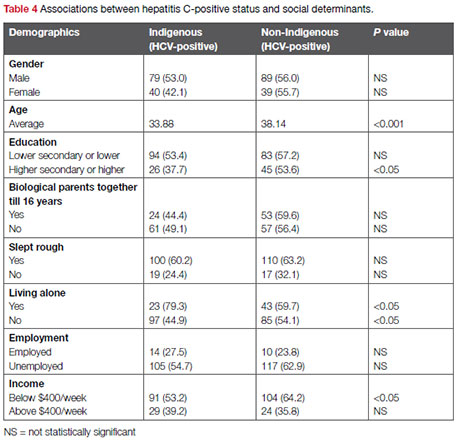
The data suggests that there are few differences between Indigenous and non-Indigenous PWID who are HCV-positive.
Where there were differences, these differences corresponded with differences in the whole sample; Indigenous HCV-positive respondents were younger, were less likely to have a higher level of education, were more likely to be living alone, and had a lower income.
Discussion
Although HCV antibody status is based on self-report, there is evidence to support its use and overall validity.8
In contrast to other studies of HCV among PWID in Australia, we did not find the Indigenous participants to be more likely to be HCV antibody positive – in fact self reported HCV infection was slightly lower among Indigenous participants (55.5% vs 61.8%).
Instead, significant differences in reported HCV antibody positivity were most clearly reflected in key social determinant indicators such as having slept rough (61.8% vs 27.5%), being unemployed (58.7% vs 25.8%), and having been to prison (66.5% vs 38.5%).
There were no significant associations between HCV infection and either mental or physical health.
Having been diagnosed with a mental health condition or a physical health problem, or having a dual diagnosis, were similar for Indigenous and non-Indigenous respondents.
With regard to drug use, it is interesting to note that while the sharing of needles and syringes in the last month was more common among Indigenous respondents (35.6% vs 18.9%), this did not translate to greater levels of HCV infection – with a prevalence of 58.1% among Indigenous PWID who had shared in the past month compared to 67.5% prevalence among non-Indigenous PWID who had shared.
We suggest that HCV infection for both Indigenous and non-Indigenous PWIDs is grounded in a complex interface of social disadvantage, social capital and risk behaviours.
This is a population existing very much at the margins of society with nearly half the population having been to prison, three out four people without employment and two thirds having an average weekly income of below $400.
Yet within this context the Indigenous participants demonstrate greater social capital. They were significantly less likely to have slept rough in the past (63.6% vs 73.3% p<0.05) and almost three times more likely to be living with others (10.8% vs 30.5%), suggesting Indigenous respondents were more likely to be in a relationship.
Strategies that simply focus on reducing risk behaviour without at least acknowledging the broader social context within which PWID live and interact will only have a limited effect – a more sustainable approach needs to account for and respond to the broader social determinants of health.
Conclusion
This is one of the few studies of injecting drug use with a substantial sample of Indigenous respondents.
This study demonstrates a remarkable homogeneity in responses from both Indigenous and non-Indigenous people who inject drugs.
In contrast to other studies looking at social disadvantage, where findings indicate Indigenous status to be a significant predictor to greater social disadvantage, this study finds both the Indigenous and non-Indigenous respondents experience high and similar levels of social disadvantage.
Patterns of drug use were similar among both Indigenous and non-Indigenous PWIDs, with Indigenous respondents more likely to be injecting amphetamines in the recent six months.
The relatively easier access to amphetamines might have contributed to amphetamines being nominated by both groups as the drug most injected in the last six months.
Drug dependence was high in both groups, with recent heroin injection significantly associated with dependence.
Non- Indigenous respondents were more likely to have experienced an overdose; this could be due to their increased use of opiates over their Indigenous counterparts.
Hepatitis C with its manifestations is an important public health issue because of its potential to increase health care costs.
Of the three most common blood borne viruses among people who inject drugs (hepatitis B, hepatitis C and HIV), HCV is the most prevalent.
The results from QuIDS suggest that Aboriginal or Torres Strait Islander status is relatively unimportant in the transmission of HCV.
Consistent with other literature for similar populations, our results demonstrate the significant association that age, homelessness, loneliness, unemployment, income and imprisonment have with a HCV-positive status.
Queensland injecting drug survey (QuIDS) Project Team
Project Advisory Group: Coralie Ober, Jake Najman, Andrew Young (University of Queensland), Robert Kemp (University of Queensland), James Ward (Baker Institute IDI, Central Australia), Vanessa Gela (Queensland Injectors Health Network), Sidney Williams (Queensland Aboriginal Health Council)
Chief Investigators: Jake Najman, Sidney Williams, James Ward, Robert Kemp Associate
Investigators: Andrew Conroy, Abhi Dev, and Suzanna Henderson.
Further information about the Queensland injecting drug survey is available at: www.uq.edu.au
Author notes
1 Queensland Health, Brisbane;
2 Baker IDI, Central Australia, Alice Springs;
3 University of Queensland, Brisbane; and
4 Queensland Aboriginal & Islander Health Council, Brisbane
References
1 National Centre in HIV Epidemiology and Clinical Research (NCHECR). (2009). Return of Investment 2: Evaluating the cost-effectiveness of needle and syringe programs in Australia. NCHECR, The University of New South Wales, Sydney.
2 Hepatitis C virus projections working group. (2006). Hepatitis C virus projections working group: Estimates and projections of the hepatitis C virus epidemic in Australia 2006. NCHECR, The University of New South Wales, Sydney.
3 Australian Government Department of Health and Ageing (DoHA). (2005). National hepatitis C strategy 2005–2008. DoHA, Canberra
4 NCHECR, op. cit.
5 Australian Institute of Health and Welfare (AIHW). (2007). Statistics of drug use in Australia 2006. AIHW, Canberra.
6 Resnick, I., Brener, L. (2010). Hepatitis C and the Aboriginal population. Social Research Briefs, 16. National Centre in HIV Social Research, Sydney, 1–4.
7 The Australian Needle and Syringe Program Survey (ANSPS) National Data Reports are available at www.kirby.unsw.edu.au
8 van der Poorten, C., Kenny, D., George, J. (2008). Prevalence of and risk factors for hepatitis C in Aboriginal and non-Aboriginal adolescent offenders. The Medical Journal of Australia, 188(10), 610–614.

